
November 23, 2022 — As the holiday season approaches, revenue forecasts for both retailers and restaurateurs — as well as the number of claims they may need to manage with less support — are on the rise. Another familiar behavior that increases at this time of the year is consumer generosity. According to Nonprofits Source, two-thirds of the U.S. population (69%) say they donate to charitable causes, and 30% of annual giving occurs in the month of December.1
The holidays provide time to reflect on past events, make plans for future improvement, and remind us that having empathy for one another can truly improve the lives of those in our community and the greater world. With the season of giving upon us, how can claims professionals work to incorporate more compassion into the claims process?
Making the dining or shopping experience pleasant leads to increased customer satisfaction and repeat business for restaurants and retailers, and we can approach claims the same way (without the desire for repeat business, of course). I have written before about the importance of aligning restaurant/retail brand culture and your claims professionals by treating the claims-handling entity as an extension of the risk management department to maintain integrity.
With only one chance to make a first impression, how businesses respond to an injury during the initial stages sets the tone for the entire claims process, including both total cost and claim duration. Conducting the claims process with empathy and compassion can support business goals and encourage brand loyalty even after an incident has been resolved. The techniques outlined below are employed differently depending on whether you are dealing with guest liability claims or associate injury claims, but in both cases, the techniques are designed to promote compassion within your extended workforce
Best Practices for Liability Claims
When a guest is injured while on premises, how we react to the incident when it is reported is vitally important to how this potential claim develops.
Start from a Place of Empathy
Once an incident is reported, meet the injured person where they are; they have suffered and are most interested in being recognized, not dismissed. Businesses should make every attempt to clearly communicate their desire to amicably resolve the situation without a statement or admission of fault.
Ensure Timely Incident Report
The expectations you set with the guest cannot be met unless the claim is reported in a timely manner to your claims administrator. During the holidays, the increased volume of guests is likely to slow down the claim-reporting process, as it might take a back seat to managing your operations. The manager on duty should use their own incident reporting protocols immediately upon receiving notice in order to document exactly what happened without losing any essential details. The documentation should include when and where the event happened, witnesses to the incident, the condition of the surrounding physical location, etc. Be sure to include pictures, if possible, to corroborate evidence of the account.
Explore Immediate Resolution Through Gift Cards
Repeat customers that share their positive experiences with friends and family are what make a business sustainable. Gift cards can also work to increase revenue (based on the fact that 65% of gift card recipients spent 38% more than the face value of their cards) and lower claims costs. Oftentimes an empathetic approach (without admitting fault) and the offer of a gift card can expedite resolution.
Set Expectations for Guest Follow-up
Setting a guest's expectations for what comes next in the claims process is vital. When they know what is going to happen and when, it may reduce the likelihood they will secure legal representation, prolonging claim duration and potentially increasing costs. At the very least, they should be informed that the company's claims handling representative will contact them within a few days and that they should reach out to a specific person with any additional questions.
Best Practices for Workers' Compensation Claims
When a claims administrator makes initial contact with the injured team member or associate, beyond showing compassion, the claims professional should proactively provide information regarding what to expect during the life of the injury event. Risk Managers and broker claims consultants need to work with their claims providers to ensure essential decisions are made and the right resources are deployed at the right time to ensure the person returns to full health as quickly as possible.
Point of Injury Nurse Triage
Implement a nurse triage program to get the injured associate speaking to a nurse immediately after the injury occurs so that the associate has a direct connection to their path to recovery. This protocol has multiple benefits, including:
- Clinical assessment of the injury to determine whether outside medical treatment is appropriate.
- If the injury can be treated as self-care, then no claim is reported against your loss run.
- If treatment is necessary, channeling away from emergency rooms to high performing network providers adhering to evidence-based medicine.
Employee Advocacy
An advocacy program — whether employer sponsored or claim-handler sponsored — is needed to provide the upfront compassion and information needed to guide an injured team member through the claims process. A simple call from the employer or outreach via text from the claims administrator to the injured worker immediately after the injury occurs can put the team member at ease and reduce the likelihood of lawyer involvement.
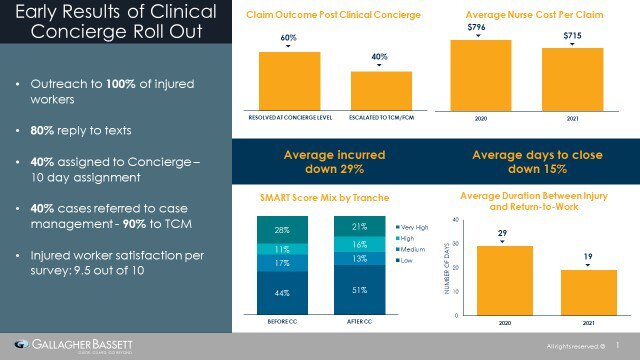
Through our GB Clinical Concierge service, a nurse reaches out to the injured worker upon receipt of the first report. This initial outreach is via text message, and it often takes place before the Resolution Manager makes their first contact. For injured workers at risk, a Concierge will be assigned to the claim for the first 10 days. The Concierge nurse is a clinical advocate who partners with the injured worker to navigate their medical engagement plan and focus on their individual barriers to recovery. At the end of the 10-day assignment, an assessment is made to determine ongoing clinical support needs. In most cases, the Concierge has positioned the injured worker for a successful recovery and will close their assignment without further intervention. For those injured workers who need additional clinical help moving forward, the appropriate GBCARE nurse case manager will be assigned to navigate their ongoing barriers to recovery and the return to work.
Claim Handler Contact and Ongoing Communication
Ultimately, the injured associate is going to have direct communication with the claim handler. It is essential that this communication be prompt and efficient. In today's technology age, an app-based communication system should be available to allow injured workers to communicate electronically. Common functionalities of these app-based systems include:
- Temporary total disability (TTD) payment history.
- Uploading of return-to-work slips from medical professionals.
- A network provider search tool.
Ongoing Assistance from Nurse Case Management
Most claims can be resolved without an ongoing clinical resource. For claims requiring a clinical resource, it should be a goal-oriented assignment to address the barriers to recovery and the return to work. When using clinical resources, it is vital that there is an individual and data-driven rationale for employing this resource. Guidelines for clinical intervention should include:
- Following best practices for clinical referral, including injury severity, biopsychosocial risk factors, and AI decision support.
- Prioritizing telephonic case management (TCM) and limiting field case management (FCM) for catastrophic and complex cases where provider quality or injured worker cooperation are risk factors.
- Acting quickly with early identification of risk factors to promote appropriate care as opposed to reacting to a problem after the care is underway.
- Leveraging AI to identify ongoing risk and opportunity for intervention as treatment progresses.
Gallagher Bassett's AI decision support tool, Clinical Guidance, measures underlying risk factors that would benefit from a nurse case manager for the first year of the claim. A complementary tool to Clinical Concierge insight, it will identify emerging risk as the claim develops. In addition to review of the injured worker risk profile, it also uncovers treatment quality risk through our ODG compliance tool, Treatment Quality Index (TQI).
As the volume of claims increases toward the end of the calendar year, it is essential that restaurant/retail businesses' internal infrastructure and claims handling partners adequately prepare to successfully manage claims. We encourage you to consult the techniques and tools outlined above to increase compassion and empathy in your advocacy efforts. This mindset will lead to long-term benefits for your injured guests and team members as well as for your business. Additionally, it can also reap rewards well into the future as your actuaries look at decreased future development.
Source
Make Gallagher Bassett your dependable partner
When making the right decision at the right time is critical to minimize risk for your business, count on Gallagher Bassett's extensive experience and global network to deliver.

